Dental implants are a special device meant to securely hold removable dentures or permanent teeth replacements in the jawbone. They are a safe and esthetically desirable replacement for missing teeth lost as the result of dental trauma or periodontal disease. The placement of implants is often preferable compared to the use of fixed dental bridges or removable full or partial dentures. According to the National Institutes of Health, there is an intimate relationship between the masticatory apparatus and the cranium and cervico-scapular muscular system. Improper occlusal positioning resulting from missing teeth may result in headaches, neck pain, or pain in and around the temporomandibular joint. Cosmetics aside, dental implants may help optimize chewing and neuromuscular occlusion. By eliminating the bacteria-friendly surface where an opposing mandibular or maxillary tooth may come into contact with the site of a missing tooth, implants mitigate the effects of TMJ disorders and reduce the risk of bone loss in the jaw caused by the onset of periodontal disease.
Patients with missing teeth who wish to consider an implant should always consult a licensed dental care provider to determine if they are an ideal candidate for this procedure. Implants may be placed by general dentists with training and experience. In more complex cases, a patient may be better suited to having an implant placed by a dental specialist such as an oral surgeon, prosthodontist, or periodontist. The entire process of replacing a missing tooth with an implant and crown may be as long as 6 months, so it is imperative for both the provider and patient to feel comfortable with the time commitment necessary to successfully complete the procedure.
An implant is a small metal cylinder, most commonly made of titanium. Ceramic implants made from zirconium have been increasing in popularity, but they are not as durable as titanium and thus have a higher failure rate. Dental implants are inserted into the jawbone in a surgical procedure, and the patient may prefer the use of local or general anesthesia to minimize pain. The size of a dental implant is measured in diameters and typically ranges from 3.5 mm to 4.2 mm for anterior teeth and 4.5 to 6 mm for posterior teeth. The dental provider should carefully evaluate each individual patient and determine the ideal implant size before initiating the surgical process.
The most common types of dental implants are endosteal and subperiosteal implants. Endosteal implants are typically used in patients with adequate bone structure and no special complications. Subperiosteal implants are used in patients with weaker jawbone structure or minimum jawbone height that is not adequate to support an endosteal implant. This may be an ideal alternative to the use of dentures. Subperiosteal implants are fitted over a patient’s jawbone and supported by a surrounding metal framework as opposed to being inserted into the jawbone. After the gums and surrounding jawbone heal, subperiosteal implants are fitted with a crown resembling a natural tooth. Following the placement of a subperiosteal implant, a dentist may even recommend the use of a removable prosthesis in the form of a crown or denture. A removable prosthesis is often a metal frame that can be secured by the abutment, and it is less expensive than a permanent prosthesis.
Endosteal implants are usually performed in four phases: planning, insertion of the implant in the jawbone, insertion of the abutment, and attachment of the crown. We will elaborate on this procedure since endosteal implants are most commonly used. During the planning phase, the dental provider conducts a thorough examination of the mouth and instructs the assistant to take dental X-rays and create a dental impression of the future site of implant placement. In addition to the examination, the dental provider will comprehensively evaluate the patient’s medical history, medical conditions, and document all medications the patient is currently taking.
If there is inadequate bone structure in the jaw to accommodate an endosteal implant, the patient and dentist may discuss the possibility of a bone graft. The bone graft may be performed by an oral surgeon if the dentist believes that a specialist would be ideally suited to performing the procedure. The bone graft may utilize biocompatible synthetic bone material or bone tissue from the patient’s own body to strengthen the jawbone.
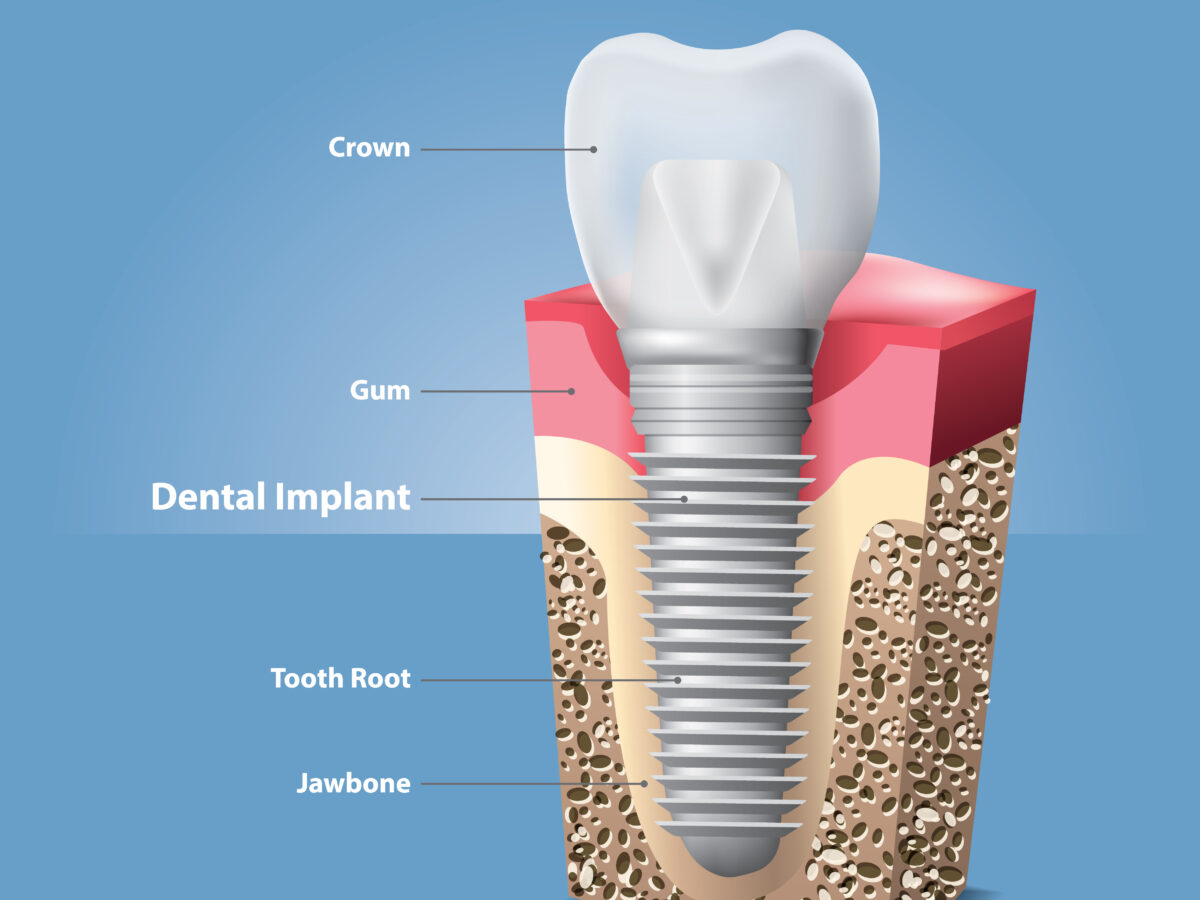
During the insertion of the implant, the patient usually presents to the dentist office for a surgical procedure. In exceptional cases, the implant procedure may be done as an outpatient procedure in a hospital setting. Following the administration of anesthesia, the dentist makes an incision in the gums to expose the jawbone. Once the appropriate amount of jawbone structure is exposed, the dentist will drill into the jawbone and create a void which will hold the implant. The provider will drill just enough to accommodate the implant that is the ideal size for the particular tooth being replaced. The implant is screwed into the patient’s jawbone, and the gum tissue is closed with absorbable or nonabsorbable sutures. This leads to the process of healing. The healing process is officially referred to as osseointegration, where the jawbone heals and fully bonds to the surrounding implant. During the healing phase, a patient may use a temporary removable denture to resemble an actual tooth. The healing process may take up to 6 months, depending on the patient.
Following the placement of the implant, an abutment is commonly placed on top of the implant cylinder. The abutment may be placed immediately after the implant or done as a second surgical procedure following the implant. The dentist will determine which sequence is ideal based on the conditions of the individual patient and the respective tooth being replaced. The abutment will be visible during the healing period. Upon placement of the abutment, the gum tissue is sutured and the top of the abutment will be visible above the gum line. The healing process following the placement of the abutment typically takes a few weeks.
Once the healing process is complete, the dentist will proceed to insert a false tooth, also known as a crown. A customized impression of the abutment area and the surrounding teeth is taken, and the impression is sent to a laboratory of the dentist’s choosing. The laboratory subsequently manufactures the prosthesis according to the provider’s specifications. The making of a crown is both science and art, and a ceramist in the lab is responsible for this task. Modern dentistry places a great deal of emphasis on cosmetics, and there is an array of corresponding colors to choose from. It is even possible to stain, glaze, and bake a crown to be virtually indistinguishable from a natural tooth and unrecognizable to others that the patient has a dental implant. Once a dental crown is made according to the custom needs of the patient, the prosthesis is permanently cemented onto an abutment. Patients should carefully choose a dental provider based on their prior experience in implant placements as well as cosmetic outcomes.
With proper care, dental implants may last several decades or even a lifetime. However, there is always a risk of side effects and complications following implant surgery. Common side effects include swelling and bruising of the gums and face, pain, bleeding, and stiff facial muscles. Less common complications may involve an infection around the site of the implant, damage to nearby teeth or blood vessels, and nerve injury. A panoramic X-Ray is a valuable diagnostic tool, and a dentist should thoroughly evaluate the positioning of sinuses and/or the positioning of the inferior alveolar nerve to minimize the possibility of sinus infection or nerve injury. If the inferior alveolar nerve is damaged, the patient may experience a loss of sensation in the gums, lips, and cheeks. In rare cases, the process of osseointegration may fail and the jawbone may not close properly around the implant cylinder. If the implant cylinder is loose due to poor placement or placement of an endosteal implant in a patient who may not be an ideal candidate, the implant must be removed and the surgical process needs to be repeated after the bone has healed.
Following the placement of an implant, patients are advised to care for implants as natural teeth and keep the surrounding gum area clean by regularly brushing and flossing. Immediately after surgery, patients should eat a diet consisting of soft foods. Upon healing, patients should avoid hard foods such as candy and jawbreakers which may crack the implant crown. If a patient experiences bruxism, they should consider using a mouthguard to minimize the possibility that the implant crown will break. All patients are advised to abstain from chewing tobacco or smoking because tobacco can stain teeth and smoking can injure the gum structure.
Dental implants are most useful for patients who do not wish to use partial or full dentures who are in good oral health. If patients have a condition that impedes healing or do not have enough bone tissue to anchor an implant, the only option to replace missing teeth may be the use of a removable denture. With recent advancements in dentistry, implants are usually an ideal choice for replacing missing teeth, and long-term success is contingent on the selection of an experienced dental provider and a patient’s commitment to maintaining optimal oral health.
What is PIP? (2 pages)
PIP stands for personal injury protection. PIP is a mandatory component of auto insurance policies that covers medical treatments for injuries resulting from auto accidents. In New Jersey, all motorists are required to carry a minimum of $15,000 PIP coverage up to a maximum of $250,000. However, if a patient has a traumatic brain or spinal cord injury, these limits may not be applicable pursuant to court settlements. Beyond liability insurance coverage paid by the liable party’s insurance company, PIP insurance covers funeral expenses, home health care, and physical therapy. While coverage mandates may vary by state, a New Jersey motorist’s PIP coverage may even be applicable if they are injured by another vehicle as a passenger or pedestrian. If a motorist has health insurance in addition to auto insurance, they have the option to choose between PIP Primary and PIP Secondary coverage. Motorists without adequate health insurance may only choose PIP Primary coverage.
For motorists with PIP Primary coverage, the insurer is primarily responsible for paying for the cost of medical treatments resulting from an auto accident after the deductible is satisfied. For motorists with PIP Secondary coverage, their auto insurance policy only covers health care expenditures beyond the scope of their health insurance coverage after all deductibles have been satisfied. Since annual deductibles continue to rise for most health insurance policies while limiting provider networks and the types of treatments that are covered, injured patients with PIP Secondary coverage typically fare worse. The modest cost savings on auto insurance premiums are almost always superseded by the cost of insurance deductibles and out-of-pocket expenses following an accident. Based on his experience working with personal injury attorneys and advocating on behalf of patients suffering from TMDs, Dr. Federman strongly recommends all motorists carry adequate PIP coverage above the state minimum and elect PIP Primary coverage.
TMJ injuries may result from whiplash or facial trauma in an auto accident, including hyperflexion or hyperextension. Following a traumatic injury, TMDs may manifest in the form of joint pain, ear pain, chronic headaches, neck pain, shoulder pain, or even difficulty opening and closing the mouth. Patients who continue to suffer long-term pain following facial trauma may not even be aware of the root cause of their impairments.
Please contact our office immediately if you believe that you have experienced facial trauma or have TMJ symptoms resulting from facial trauma. If a patient needs TMJ treatment, physical therapy, or surgery as the result of an accidental injury resulting from the negligence of another person or party, personal injury protection (PIP) insurance or workers compensation will likely cover most or all of the cost of treatment. Dr. Federman and his associates have a terrific relationship with the most prominent injury lawyers in the community, along with a thorough understanding of the laws regulating insurance payouts. We will work diligently on behalf of all injury patients to ensure that cost will not be a barrier to receiving TMJ treatments and all necessary rehabilitative care.
During the initial evaluation, Dr. Federman and his staff will evaluate the patient’s overall condition, lifestyle choices, and goals for long-term treatment and recovery. Patients should not hesitate to ask questions. This step is crucial in determining whether or not the patient is a candidate for TMJ treatment in particular. Upon evaluating the patient and reviewing all medical records, he will develop a multifaceted treatment plan tailored to each individual patient.
To maximize the likelihood of a successful treatment, it is important for patients to be fully committed to following the treatment plan and lifestyle modifications recommended by our doctor. With personalized care to suit the needs of each TMJ patient, our primary goal is to ameliorate our patients’ quality of life through the most minimally invasive treatment possible. If you are interested in learning more about our TMJ treatments, please contact Dr. Federman’s office to schedule a consultation.